Frontotemporal Dementia
What is Frontotemporal Dementia?
Frontotemporal dementia (FTD) is a group of brain disorders caused by the gradual loss of nerve cells in the frontal and temporal lobes. It accounts for around 15% of all dementia cases and typically affects individuals under the age of 65 years, although it can occur at any age. FTD affects both men and women equally.
What Happens in Frontotemporal Dementia?
The symptoms of frontotemporal dementia (FTD) depend on the specific regions of the brain that are impacted. The frontal lobes are crucial for planning, social behaviour, speech production, and decision-making. The temporal lobes are essential for language comprehension and conceptual understanding. With pathological changes taking place in these brain regions, individuals may experience a range of symptoms, including alterations in cognitive abilities, shifts in personality, difficulties in language skills, or impairments in movement and coordination. Recognising these symptoms is vital for early diagnosis and intervention, understanding of the condition's progression and potential strategies for management.
Types of Frontotemporal Dementia
FTD can present in different ways, depending on which brain regions are primarily affected. The three main clinical presentations are:
-
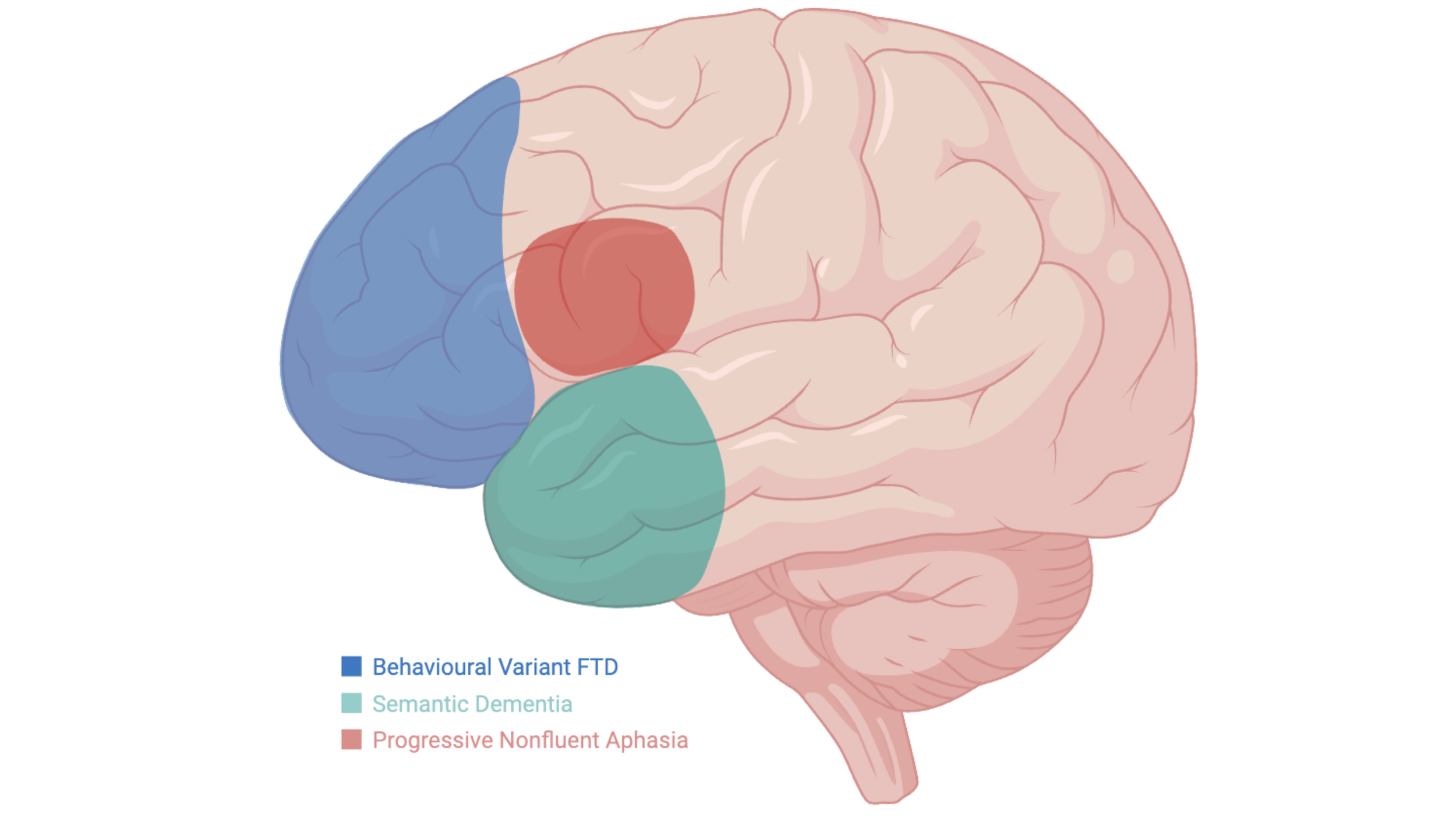
This is the most common presentation of frontotemporal dementia. It predominantly affects the frontal lobes of the brain bilaterally (blue regions in the figure), leading to changes in personality and behaviour. Individuals with bvFTD may become impulsive, socially inappropriate, apathetic (less motivation or initiative), or emotionally detached. They may also show reduced empathy and poor judgement.
-
Semantic dementia primarily affects the anterior portion of the temporal lobes (green region in the figure). The left temporal lobe is generally more affected than the right, although the opposite pattern is found in some individuals. Individuals may have fluent speech but struggle to understand words, forget object names, or fail to recognise familiar things.
-
Progressive nonfluent aphasia primarily affects the left inferior frontal lobe (red region in the figure). This brain region is responsible for speech production. Speech becomes slow and effortful, and individuals may struggle to form sentences or pronounce words clearly.
These presentations are caused by different underlying brain pathologies but share a common feature: they primarily affect the frontal and temporal regions of the brain. Over time, the brain pathology will progress to involve other brain regions as well.
In the literature, these presentations may be referred to by their specific names or collectively as frontotemporal dementia. In addition, semantic dementia and progressive nonfluent aphasia are also classified as variants of primary progressive aphasia (PPA), as their symptoms primarily involve the breakdown of language skills. In this context, these subtypes are also referred to as the semantic variant (svPPA) and nonfluent variant (nfvPPA) of primary progressive aphasia.
Types of Frontotemporal Dementia
In some instances, movement disorders may be present alongside FTD. These presentations include motor neuron disease (MND), corticobasal syndrome (CBS), or progressive supranuclear palsy (PSP). CBS and PSP are sometimes referred to as Parkinson’s-plus syndromes.
Clinicians and researchers often use the term frontotemporal lobar degeneration (FTLD) to describe this broader family of conditions. FTLD includes the main FTD subtypes—bvFTD, SD, and PNFA—as well as the movement-related conditions—CBS, PSP, and FTD-MND. These conditions are grouped together because they share similar underlying brain changes, including the build-up of FTD-related abnormal proteins (such as tau or TDP-43). See Pathology for more information.
Some Common Questions About frontotemporal dementia
Diagnosing FTD involves several steps:
Medical history and symptom review: Diagnosis often starts when changes in behaviour, speech, or thinking are noticed by the individual or their loved ones, leading to a visit to the GP.
Referral to specialists: Specialists such as neurologists or geriatricians perform detailed assessments. This includes gathering information from family or carers to understand how symptoms have developed over time.
Cognitive testing: Neuropsychological tests measure memory, language skills, problem-solving, and social behaviour to pinpoint which thinking abilities are affected.
Brain imaging and blood tests: MRI or PET scans help identify changes in the brain’s structure and activity. Blood and spinal fluid tests may also be used to identify the pathological ‘signature’ of the dementia or rule out other causes for the presentation.
How is Frontotemporal Dementia Diagnosed?
If you or someone close to you is experiencing changes that raise concerns about FTD, the first step is to speak with your GP. They will assess your symptoms and, if appropriate, refer you to a specialist for further evaluation.
If you have already had some investigations and would like input from our team, please visit Get Involved to find out more.